The Predictive Value of Second-Look Ultrasound after Preoperative Breast Magnetic Resonance Imaging
Article information
Abstract
Purpose:
The purpose of the current study was to evaluate the usefulness of second-look ultrasonography (US) for evaluating incidental enhancing lesions identified on preoperative breast magnetic resonance imaging (MRI) performed to stage malignant lesions.
Methods:
We studied 88 patients with suspected breast malignancy on conventional mammography and/or whole-breast US and invasive carcinoma subsequently confirmed by cytology or core biopsy, who underwent preoperative breast MRI for accurate breast cancer staging between January 2011 and July 2014. Patients’ demographic, clinical and pathological characteristics were assessed.
Results:
Seven hundred forty-nine patients underwent preoperative breast MRI, and the imaging detected incidental enhancing lesions in 257 patients. Second-look US was performed to evaluate 126 incidental enhancing lesions in 88 patients. We evaluated the frequency of malignancy as a function of lesion size on MRI, lesion size on second-look US, menstrual status, and age. The frequency of malignancy was higher for lesions 0.6 cm or larger on MRI than for smaller lesions (25.9% vs. 0%), and this difference was statistically significant (p=0.032).
Conclusion:
In conclusion, we found that the frequency of malignancy increased with the size of incidental enhancing lesions detected by MRI. On the basis of our results, biopsy is warranted in cases of incidental enhancing lesions 0.6 cm or larger on MRI. Further study with a larger series of cases and including more detailed subgroup analyses is necessary to develop reliable management guidelines for these lesions.
INTRODUCTION
Breast cancer is the most common malignancy in women, and invasive carcinoma of no special type is the most common form of breast cancer [1,2]. Therefore, substantial effort has been devoted to identifying factors with therapeutic significance and those that aid in the prognosis of breast cancer.
Noninvasive diagnostic imaging of breast carcinoma includes mammography (MMG), ultrasonography (US), and magnetic resonance imaging (MRI).
Breast MRI is well established as the most sensitive diagnostic tool for the detection and staging of malignant breast lesions [3]. MRI has proved particularly valuable, over whole-breast US and MMG, for detecting unsuspected multifocal disease [3]. Breast second-look US is a technique widely used in clinical practice to re-evaluate previous US findings after the acquired knowledge of additional suspicious or indeterminate lesions, previously undetected, revealed by contrast-enhanced MRI [4]. Unfortunately the detection of abnormal enhancing lesions not seen on previous MMG and whole-breast US is potentially problematic for subsequent patient-management decisions because it is sometimes unclear whether these lesions should be ignored, followed up or referred for biopsy.
The purpose of the current study was to evaluate the usefulness of second-look US for evaluting incidental enhancing lesions identified on preoperative breast MRI performed to stage malignant lesions.
METHODS
Patient selection
We studied 88 patients with suspected breast malignancy on conventional MMG and/or whole-breast US, and invasive carcinoma subsequently confirmed by cytology or core biopsy, who underwent preoperative breast MRI for accurate breast cancer staging at the Kangbuk Samsung Hospital between January 2011 and July 2014. All studies were conducted with the prior approval of the Institutional Review Board of Kangbuk Samsung Hospital (approval number: 2015-03-001). All patients underwent initial whole-breast US. No patient had undergone chemotherapy or received any other contrast material in the week prior to the breast MRI study. Patients were characterized based on their clinicopathological characteristics, such as age at diagnosis and menopausal status. Patients with incidental enhancing lesions detected on MRI subsequently underwent a second-look high-resolution US examination directed specifically at the site of the incidental finding.
Magnetic resonance imaging
All breast MRI examinations were performed using the Intera 1.5T system (Philips Medical Systems, Best, The Netherlands) and a 4-channel bilateral breast surface coil while patients were in the prone position. Temporal resolutions of dynamic imaging were used.
An intravenous bolus injection of 0.1 mmol gadobutrol (Gadovist®; Bayer HealthCare Pharmaceuticals, Berlin, Germany) or 0.1 mmol gadodiamide (Omniscan™; GE Healthcare AS, Oslo, Norway) per kilogram body weight was administered with a flow rate of 1 mL/sec followed by a 20-mL saline flush. Then, the tumor size was measured by an axial postcontrast dynamic enhancement subtraction with fat suppression, at a slice thickness of 5 mm. The lesion diameter was measured on the first or second subtracted axial images and on their sagittal and coronal reconstructions. The largest of these three diameters was considered to be a measure of the lesion’s size. Morphological analysis was reported according to the Breast Imaging Reporting and Data System (BI-RADS) classification. To avoid biased reading, all MRI images were retrospectively reviewed by two breast radiologists with at least 10 years of experience each, without US, MMG, or clinical information.
Second-look US
Ultrasonography was performed using an iU22 (Philips Healthcare, Bothell, USA) or an Aixplorer® (SuperSonic Imagine, Aix-en-Provence, France) equipped with a 12- to 5-MHz linear-array transducer. The longest tumor diameter, on the longitudinal view of US, was measured.
Lesion biopsy
All incidental enhancing lesions detected on breast MRI that were considered category 0, 3, 4, or 5 according to the BI-RADS classification and that subsequently had a suspicious correlate on second-look US (BI-RADS 4–5) were evaluated histologically immediately after the second-look US examination.
Lesions with a definite suspicious US correlate were evaluated by means of core needle biopsy under US guidance or by excisional biopsy following US-guided wire localization. Incidental enhancing lesions on brest MRI that had a correlate lesions on second-look US that was considered benign or probably benign (BI-RADS 2-3) were mananged conservatively.
Statistics
Qualitative variables were compared using Pearson chi-square test with Yates’ correction, and Fisher exact test. All tests for significance were two-tailed. All statistical analyses were performed using IBM SPSS Statistics 21.0 (IBM Corp., Armonk, USA), with statistical significance set at p < 0.05.
RESULTS
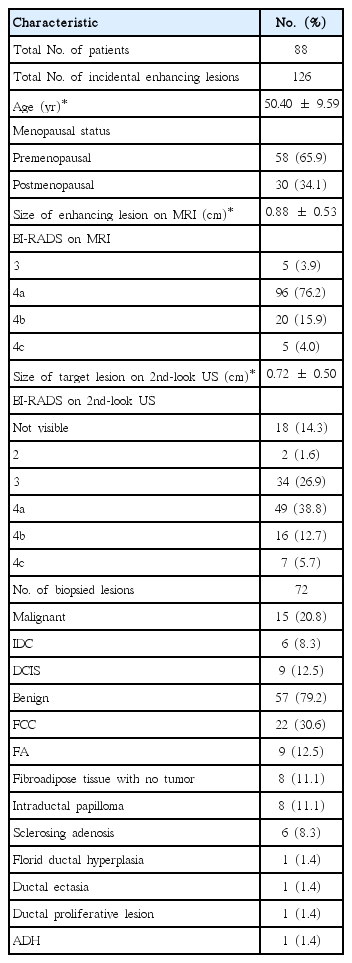
Seven hundred forty-nine patients underwent preoperative breast MRI, and the imaging detected incidental enhancing lesions in 257 patients. Of these, 169 patients with lesions classified as BI-RADS 2–3 on MRI were excluded from the study, and these patients received follow-up with breast MRI annually. Even though it was not acceptable according to our inclusion criteria, five lesions that had been classified as BI-RADS 3 on MRI were also subjected to second-look US. Because those lesions were detected while other BI-RADS 4 were being evaluated by second-look US, second-look US was also performed for those five lesions. Second-look US was performed to evaluate all 126 incidental enhancing lesions of the remaining 88 patients (Figure 1). The clinicopathological characteristics of the 88 patients are described in Table 1. All 88 patients were female and the mean age was 50.40±9.59 years. The mean size of the enhancing lesions on MRI was 0.88±0.53 cm. A total of 126 incidental enhancing lesions, classified as BIRADS 3 (n = 5), 4a (n = 96), 4b (n =20), and 4c (n = 5) on MRI, were subjected to second-look US.
Upon second-look US re-evaluation, the 126 incidental enhancing lesions were re-classified as BI-RADS 2 (n =2), BI-RADS 3 (n =34), 4a (n = 49), 4b (n =16), 4c (n =7), and not visible (n =18).
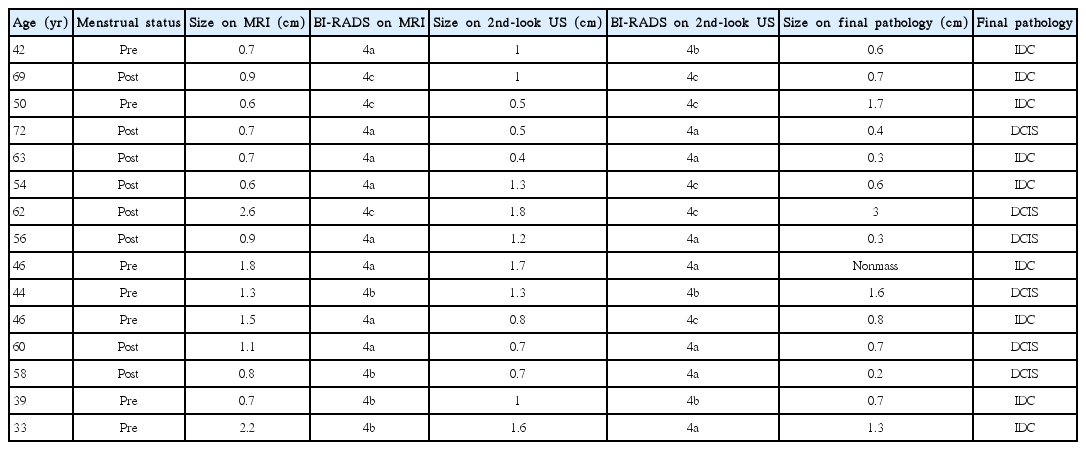
The 72 lesions classified as BI-RADS 4a, 4b, and 4c on second-look US were biopsied and 15 were histologically confirmed as malignant, while 57 were confirmed as benign (Table 1). Clinical and pathologic characteristics of the patients with histologically confirmed malignancy are described in Table 2. We evaluated the frequency of malignancy as a function of (1) lesion size on MRI; (2) lesion size on second-look US; (3) menstrual status; and (4) age.
Influence of lesion size on MRI
Of 14 lesions that were smaller than 0.6 cm, no lesion was confirmed as malignant. Of 58 lesions that were larger than 0.6 cm, 15 lesions were confirmed as malignant. The frequency of malignancy was higher for lesions 0.6 cm or larger than for smaller lesions (25.9% vs. 0%), and this difference was statistically significant (p = 0.032). The frequency of malignancy was the same for lesions 1.0 cm or larger as for smaller lesions (20.6% vs. 20.9%); the difference was not statistically significant (p = 0.980) (Table 3).
Influence of lesion size on second-look US
Of 20 lesions that were smaller than 0.6 cm, three lesions were confirmed as malignant. Of 52 lesions that were larger than 0.6 cm, 12 lesions were confirmed as malignant. The frequency of malignancy was higher for lesions 0.6 cm or larger than for smaller lesions (23.1% vs. 15.0%), although this difference was not statistically significant (p = 0.534). The frequency of malignancy was also higher for lesions 1.0 cm or larger than for smaller lesions (31.0% vs. 13.9%), and this difference was also not statistically significant (p = 0.080) (Table 3).
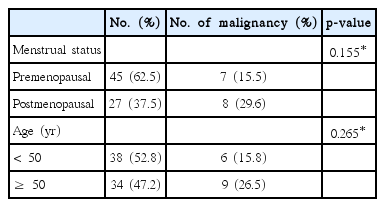
Influence of menstrual status
The frequency of malignancy was higher in postmenopausal patients than in premenopausal patients (29.6% vs. 15.5%), although this difference did not reach statistical significance (p = 0.155) (Table 4).
Influence of age
The frequency of malignancy was higher in patients 50 years or older than in younger patients (26.5% vs. 15.8%), although this difference was not statistically significant (p = 0.265) (Table 4).
DISCUSSION
Breast MRI has been widely known for its high sensitivity for detecting lesions in breast cancer [5-8]. However, when incidental enhancing lesions are detected on MRI that had previously gone undetected on conventional MMG or US, second-look US is considered next step for evaluating these lesions.
In the current study, we evaluated the utility of second-look US for incidental enhancing lesions on MRI and evaluated factors that are correlated with a high detection rate of malignancy.
In our study, 126 incidental enhancing lesions, considered BIRADS 3, 4a, 4b, or 4c on MRI, were detected in 88 patients referred for preoperative breast MRI for histologically confirmed breast cancer depicted on MMG and/or first-look whole breast US. A second-look US correlate was observed for the 126 lesions.
We studied the association between lesion size on MRI, lesion size on second-look US, menstrual status, age, and the frequency of malignancy for 126 lesions. To our knowledge, there has been no previous study evaluating the relationship between age, menstrual status, and frequency of malignancies for incidental enhancing lesions on MRI. However, age and menstrual status are closely related to incidence of breast cancer, so we included those factors in the current study. In this study, both variables were not significant factors (Table 4).
Based on the result of a previous study, lesion size was significantly correlated with the frequency of malignancy [9]. In our results, the detection rate of malignancy was found to be higher only in patients with enhancing lesion 0.6 cm or larger on MRI (Table 3). We set the cutoff value for lesion size at 0.6 cm based on the result of the previous study [9]. Since the mean age of our patients was 50.40±9.59, we set the cutoff value for age at 50 (Table 1).
The detection of incidental enhancing lesions on breast MRI influenced our surgical plans. In our study, 15 patients had incidental enhancing lesions that were histologically confirmed to be malignant. Among those 15 patients, in three patients who were primarily originally scheduled to undergo breast-conserving surgery changed to mastectomy.
A study by Linda et al. [9] showed that the frequency of malignancy increased with increasing lesion size. In that study, the frequency of malignancy was significantly higher for larger lesions than for smaller lesions. In addition, Liberman et al. [10] recently demonstrated a similar trend in a large population of MRI-detected lesions without a sonographic correlate. Although our findings suggest that lesion detection on second-look US does not increase the likelihood that a lesion detected on MRI is malignant, further work in a larger patient cohort should certainly be performed to clarify these findings [11].
Previous studies have reported the utility of second-look US for incidental enhancing lesions on MRI [12,13].
The limitations of our study include the fact that it is retrospective in nature. We did not perform subgroup analyses in patients with dense breast parenchyma. In addition we did not specifically assess patients at increased familial risk of breast cancer or women with documented BRCA1 or BRCA2 gene mutations. Future prospective work should be performed to evaluate the role of second-look US specifically in women with proven or profile-like germ-line mutations.
In conclusion, we found that the frequency of malignancy increased with the size of incidental enhancing lesions on MRI. On the basis of our results, biopsy is warranted in cases of incidental enhancing lesions 0.6 cm or larger on MRI. Further study with a larger series of cases and including more detailed subgroup analyses is necessary to develop reliable management guidelines for these lesions.
Notes
The authors declare that they have no competing interests.